Artlabeling Activity Ovaries and Their Relationship to the Uterine Tubes and Uterus 1 of 2
Learning Objectives
By the end of this department, you will be able to:
- Draw the structure and function of the organs of the female reproductive system
- List the steps of oogenesis
- Describe the hormonal changes that occur during the ovarian and menstrual cycles
- Trace the path of an oocyte from ovary to fertilization
The female reproductive system functions to produce gametes and reproductive hormones, simply like the male reproductive organisation; however, information technology too has the boosted task of supporting the developing fetus and delivering information technology to the outside world. Dissimilar its male counterpart, the female person reproductive system is located primarily within the pelvic cavity. Retrieve that the ovaries are the female gonads. The gamete they produce is called an oocyte. Nosotros'll discuss the production of oocytes in item shortly. Start, permit's wait at some of the structures of the female reproductive system.
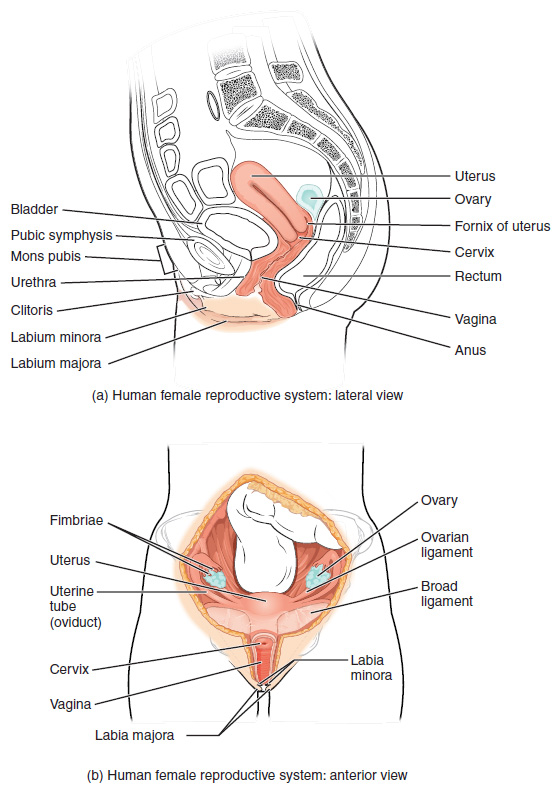
Figure 1. The major organs of the female person reproductive system are located inside the pelvic cavity.
External Female Genitals
The external female person reproductive structures are referred to collectively every bit the vulva. The mons pubis is a pad of fat that is located at the inductive, over the pubic os. Afterwards puberty, it becomes covered in pubic pilus. The labia majora (labia = "lips"; majora = "larger") are folds of hair-covered pare that begin only posterior to the mons pubis. The thinner and more pigmented labia minora (labia = "lips"; minora = "smaller") extend medial to the labia majora. Although they naturally vary in shape and size from woman to adult female, the labia minora serve to protect the female urethra and the entrance to the female reproductive tract.
The superior, inductive portions of the labia minora come together to encircle the clitoris (or glans clitoris), an organ that originates from the same cells as the glans penis and has arable nerves that get in of import in sexual sensation and orgasm. The hymen is a sparse membrane that sometimes partially covers the entrance to the vagina. An intact hymen cannot exist used as an indication of "virginity"; even at birth, this is only a partial membrane, equally menstrual fluid and other secretions must be able to exit the torso, regardless of penile–vaginal intercourse. The vaginal opening is located betwixt the opening of the urethra and the anus. It is flanked by outlets to the Bartholin'southward glands (or greater vestibular glands).

Figure ii. The external female genitalia are referred to collectively as the vulva.
Vagina
The vagina is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract. Information technology also serves as the exit from the uterus during menses and childbirth. The outer walls of the anterior and posterior vagina are formed into longitudinal columns, or ridges, and the superior portion of the vagina—called the fornix—meets the protruding uterine cervix. The walls of the vagina are lined with an outer, gristly adventitia; a center layer of smoothen muscle; and an inner mucous membrane with transverse folds called rugae. Together, the middle and inner layers allow the expansion of the vagina to adapt intercourse and childbirth. The thin, perforated hymen can partially surround the opening to the vaginal orifice. The hymen can be ruptured with strenuous physical exercise, penile–vaginal intercourse, and childbirth. The Bartholin'southward glands and the bottom vestibular glands (located almost the clitoris) secrete mucus, which keeps the vestibular area moist.
The vagina is home to a normal population of microorganisms that help to protect confronting infection by pathogenic bacteria, yeast, or other organisms that can enter the vagina. In a healthy woman, the most predominant type of vaginal bacteria is from the genus Lactobacillus. This family of beneficial bacterial flora secretes lactic acid, and thus protects the vagina by maintaining an acidic pH (below 4.v). Potential pathogens are less likely to survive in these acidic conditions. Lactic acid, in combination with other vaginal secretions, makes the vagina a self-cleansing organ. Still, douching—or washing out the vagina with fluid—tin disrupt the normal balance of healthy microorganisms, and actually increment a adult female's hazard for infections and irritation. Indeed, the American College of Obstetricians and Gynecologists recommend that women do not douche, and that they allow the vagina to maintain its normal healthy population of protective microbial flora.
Ovaries
The ovaries are the female gonads. Paired ovals, they are each about 2 to 3 cm in length, most the size of an almond. The ovaries are located within the pelvic cavity, and are supported by the mesovarium, an extension of the peritoneum that connects the ovaries to the broad ligament. Extending from the mesovarium itself is the suspensory ligament that contains the ovarian claret and lymph vessels. Finally, the ovary itself is attached to the uterus via the ovarian ligament.
The ovary comprises an outer covering of cuboidal epithelium called the ovarian surface epithelium that is superficial to a dense connective tissue covering called the tunica albuginea. Beneath the tunica albuginea is the cortex, or outer portion, of the organ. The cortex is composed of a tissue framework called the ovarian stroma that forms the bulk of the developed ovary. Oocytes develop within the outer layer of this stroma, each surrounded past supporting cells. This grouping of an oocyte and its supporting cells is called a follicle. The growth and evolution of ovarian follicles will be described shortly. Beneath the cortex lies the inner ovarian medulla, the site of claret vessels, lymph vessels, and the nerves of the ovary. Y'all will acquire more than about the overall anatomy of the female person reproductive arrangement at the end of this section.
The Ovarian Wheel
The ovarian cycle is a set of anticipated changes in a female person's oocytes and ovarian follicles. During a woman's reproductive years, information technology is a roughly 28-day cycle that can be correlated with, but is non the same every bit, the menstrual cycle (discussed shortly). The wheel includes 2 interrelated processes: oogenesis (the product of female gametes) and folliculogenesis (the growth and evolution of ovarian follicles).
Oogenesis
Gametogenesis in females is called oogenesis. The process begins with the ovarian stem cells, or oogonia. Oogonia are formed during fetal development, and divide via mitosis, much like spermatogonia in the testis. Dissimilar spermatogonia, yet, oogonia form primary oocytes in the fetal ovary prior to birth. These primary oocytes are then arrested in this phase of meiosis I, only to resume it years after, beginning at puberty and continuing until the adult female is almost menopause (the cessation of a woman's reproductive functions). The number of main oocytes present in the ovaries declines from one to 2 million in an baby, to approximately 400,000 at puberty, to zero by the stop of menopause.
The initiation of ovulation—the release of an oocyte from the ovary—marks the transition from puberty into reproductive maturity for women. From then on, throughout a woman's reproductive years, ovulation occurs approximately once every 28 days. Simply prior to ovulation, a surge of luteinizing hormone triggers the resumption of meiosis in a primary oocyte. This initiates the transition from principal to secondary oocyte. However, as y'all tin can see in Figure 3, this cell division does non result in two identical cells. Instead, the cytoplasm is divided unequally, and one daughter cell is much larger than the other. This larger jail cell, the secondary oocyte, eventually leaves the ovary during ovulation. The smaller cell, chosen the get-go polar body, may or may not complete meiosis and produce second polar bodies; in either case, information technology eventually disintegrates. Therefore, even though oogenesis produces up to four cells, only one survives.

Figure iii. Click for a larger prototype. The diff cell division of oogenesis produces i to three polar bodies that afterward dethrone, as well as a single haploid ovum, which is produced but if there is penetration of the secondary oocyte by a sperm jail cell.
How does the diploid secondary oocyte become an ovum—the haploid female person gamete? Meiosis of a secondary oocyte is completed just if a sperm succeeds in penetrating its barriers. Meiosis Ii and then resumes, producing i haploid ovum that, at the instant of fertilization past a (haploid) sperm, becomes the first diploid cell of the new offspring (a zygote). Thus, the ovum tin can be idea of as a brief, transitional, haploid phase between the diploid oocyte and diploid zygote.
The larger amount of cytoplasm contained in the female person gamete is used to supply the developing zygote with nutrients during the period betwixt fertilization and implantation into the uterus. Interestingly, sperm contribute just DNA at fertilization —not cytoplasm. Therefore, the cytoplasm and all of the cytoplasmic organelles in the developing embryo are of maternal origin. This includes mitochondria, which comprise their own Deoxyribonucleic acid. Scientific research in the 1980s determined that mitochondrial Dna was maternally inherited, meaning that you can trace your mitochondrial DNA directly to your mother, her mother, and so on back through your female person ancestors.
Everyday Connections: Mapping Human being History with Mitochondrial DNA
When we talk about human DNA, we're unremarkably referring to nuclear Deoxyribonucleic acid; that is, the DNA coiled into chromosomal bundles in the nucleus of our cells. We inherit half of our nuclear Deoxyribonucleic acid from our father, and one-half from our mother. Nevertheless, mitochondrial Deoxyribonucleic acid (mtDNA) comes just from the mitochondria in the cytoplasm of the fat ovum we inherit from our mother. She received her mtDNA from her female parent, who got it from her mother, and so on. Each of our cells contains approximately 1700 mitochondria, with each mitochondrion packed with mtDNA containing approximately 37 genes.
Mutations (changes) in mtDNA occur spontaneously in a somewhat organized pattern at regular intervals in human history. By analyzing these mutational relationships, researchers accept been able to determine that we tin can all trace our ancestry back to one adult female who lived in Africa about 200,000 years ago. Scientists have given this woman the biblical proper name Eve, although she is not, of course, the outset Homo sapiens female. More precisely, she is our nearly recent common ancestor through matrilineal descent.
This doesn't mean that anybody's mtDNA today looks exactly like that of our ancestral Eve. Considering of the spontaneous mutations in mtDNA that have occurred over the centuries, researchers tin map dissimilar "branches" off of the "main body" of our mtDNA family tree. Your mtDNA might have a pattern of mutations that aligns more closely with ane branch, and your neighbor'due south may align with some other co-operative. Still, all branches somewhen atomic number 82 back to Eve.
But what happened to the mtDNA of all of the other Homo sapiens females who were living at the time of Eve? Researchers explain that, over the centuries, their female descendants died childless or with only male children, and thus, their maternal line—and its mtDNA—concluded.
Folliculogenesis
Again, ovarian follicles are oocytes and their supporting cells. They grow and develop in a process called folliculogenesis, which typically leads to ovulation of one follicle approximately every 28 days, forth with death to multiple other follicles. The death of ovarian follicles is called atresia, and can occur at any bespeak during follicular evolution. Retrieve that, a female person infant at birth will have one to ii million oocytes within her ovarian follicles, and that this number declines throughout life until menopause, when no follicles remain. As you'll come across next, follicles progress from primordial, to primary, to secondary and tertiary stages prior to ovulation—with the oocyte inside the follicle remaining every bit a primary oocyte until right before ovulation.
Folliculogenesis begins with follicles in a resting state. These pocket-sized primordial follicles are present in newborn females and are the prevailing follicle type in the adult ovary. Primordial follicles accept only a unmarried flat layer of support cells, called granulosa cells, that surround the oocyte, and they tin can stay in this resting land for years—some until right before menopause.
After puberty, a few primordial follicles volition respond to a recruitment signal each day, and will join a pool of immature growing follicles chosen principal follicles. Primary follicles beginning with a unmarried layer of granulosa cells, only the granulosa cells then become active and transition from a apartment or squamous shape to a rounded, cuboidal shape as they increase in size and proliferate. Every bit the granulosa cells split, the follicles—at present called secondary follicles—increase in diameter, calculation a new outer layer of connective tissue, blood vessels, and theca cells—cells that work with the granulosa cells to produce estrogens.
Within the growing secondary follicle, the primary oocyte now secretes a thin acellular membrane called the zona pellucida that will play a critical role in fertilization. A thick fluid, called follicular fluid, that has formed betwixt the granulosa cells also begins to collect into one large pool, or antrum. Follicles in which the antrum has become large and fully formed are considered third follicles (or antral follicles). Several follicles achieve the tertiary stage at the same fourth dimension, and most of these will undergo atresia. The one that does not die volition continue to abound and develop until ovulation, when it will expel its secondary oocyte surrounded by several layers of granulosa cells from the ovary. Proceed in mind that nearly follicles don't brand information technology to this point. In fact, roughly 99 percent of the follicles in the ovary volition undergo atresia, which can occur at any phase of folliculogenesis.

Figure iv. Click for a larger epitome. (a) The maturation of a follicle is shown in a clockwise direction proceeding from the primordial follicles. FSH stimulates the growth of a 3rd follicle, and LH stimulates the production of estrogen by granulosa and theca cells. In one case the follicle is mature, information technology ruptures and releases the oocyte. Cells remaining in the follicle and then develop into the corpus luteum. (b) In this electron micrograph of a secondary follicle, the oocyte, theca cells (thecae folliculi), and developing antrum are conspicuously visible. EM × 1100. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Hormonal Control of the Ovarian Wheel
The process of development that we take just described, from primordial follicle to early tertiary follicle, takes approximately two months in humans. The final stages of development of a pocket-size cohort of third follicles, ending with ovulation of a secondary oocyte, occur over a course of approximately 28 days. These changes are regulated past many of the aforementioned hormones that regulate the male reproductive system, including GnRH, LH, and FSH.
As in men, the hypothalamus produces GnRH, a hormone that signals the anterior pituitary gland to produce the gonadotropins FSH and LH. These gonadotropins leave the pituitary and travel through the bloodstream to the ovaries, where they bind to receptors on the granulosa and theca cells of the follicles. FSH stimulates the follicles to abound (hence its name of follicle-stimulating hormone), and the 5 or half dozen tertiary follicles expand in diameter. The release of LH too stimulates the granulosa and theca cells of the follicles to produce the sex steroid hormone estradiol, a blazon of estrogen. This phase of the ovarian bike, when the 3rd follicles are growing and secreting estrogen, is known as the follicular stage.
The more granulosa and theca cells a follicle has (that is, the larger and more developed information technology is), the more estrogen it will produce in response to LH stimulation. As a result of these large follicles producing large amounts of estrogen, systemic plasma estrogen concentrations increase. Following a classic negative feedback loop, the high concentrations of estrogen will stimulate the hypothalamus and pituitary to reduce the product of GnRH, LH, and FSH. Because the large tertiary follicles crave FSH to grow and survive at this point, this decline in FSH caused by negative feedback leads most of them to die (atresia). Typically merely one follicle, now called the ascendant follicle, will survive this reduction in FSH, and this follicle will exist the one that releases an oocyte. Scientists have studied many factors that lead to a item follicle becoming dominant: size, the number of granulosa cells, and the number of FSH receptors on those granulosa cells all contribute to a follicle becoming the 1 surviving dominant follicle.

Effigy 5. Click for a larger image. The hypothalamus and pituitary gland regulate the ovarian bike and ovulation. GnRH activates the anterior pituitary to produce LH and FSH, which stimulate the production of estrogen and progesterone by the ovaries.
When only the one dominant follicle remains in the ovary, it again begins to secrete estrogen. It produces more estrogen than all of the developing follicles did together before the negative feedback occurred. It produces and then much estrogen that the normal negative feedback doesn't occur. Instead, these extremely high concentrations of systemic plasma estrogen trigger a regulatory switch in the anterior pituitary that responds by secreting big amounts of LH and FSH into the bloodstream. The positive feedback loop past which more estrogen triggers release of more LH and FSH only occurs at this point in the cycle.
It is this large flare-up of LH (called the LH surge) that leads to ovulation of the ascendant follicle. The LH surge induces many changes in the ascendant follicle, including stimulating the resumption of meiosis of the chief oocyte to a secondary oocyte. As noted earlier, the polar body that results from unequal cell partition simply degrades. The LH surge also triggers proteases (enzymes that cleave proteins) to intermission down structural proteins in the ovary wall on the surface of the bulging dominant follicle. This degradation of the wall, combined with pressure from the large, fluid-filled antrum, results in the expulsion of the oocyte surrounded by granulosa cells into the peritoneal cavity. This release is ovulation.
In the next section, you will follow the ovulated oocyte as it travels toward the uterus, merely there is ane more important event that occurs in the ovarian bike. The surge of LH also stimulates a change in the granulosa and theca cells that remain in the follicle after the oocyte has been ovulated. This alter is chosen luteinization (recall that the full name of LH is luteinizing hormone), and information technology transforms the collapsed follicle into a new endocrine structure called the corpus luteum, a term significant "yellow torso". Instead of estrogen, the luteinized granulosa and theca cells of the corpus luteum brainstorm to produce large amounts of the sex steroid hormone progesterone, a hormone that is critical for the establishment and maintenance of pregnancy. Progesterone triggers negative feedback at the hypothalamus and pituitary, which keeps GnRH, LH, and FSH secretions low, then no new dominant follicles develop at this time.
The postal service-ovulatory phase of progesterone secretion is known as the luteal stage of the ovarian wheel. If pregnancy does not occur within 10 to 12 days, the corpus luteum will stop secreting progesterone and degrade into the corpus albicans, a nonfunctional "whitish trunk" that will disintegrate in the ovary over a period of several months. During this time of reduced progesterone secretion, FSH and LH are once again stimulated, and the follicular phase begins again with a new cohort of early on tertiary follicles beginning to grow and secrete estrogen.
The Uterine Tubes
The uterine tubes (also called fallopian tubes or oviducts) serve every bit the conduit of the oocyte from the ovary to the uterus. Each of the two uterine tubes is close to, but not directly connected to, the ovary and divided into sections. The isthmus is the narrow medial end of each uterine tube that is continued to the uterus. The wide distal infundibulum flares out with slender, finger-like projections chosen fimbriae. The middle region of the tube, called the ampulla, is where fertilization ofttimes occurs. The uterine tubes also take three layers: an outer serosa, a centre smoothen muscle layer, and an inner mucosal layer. In addition to its fungus-secreting cells, the inner mucosa contains ciliated cells that beat in the management of the uterus, producing a current that will be disquisitional to move the oocyte.
Following ovulation, the secondary oocyte surrounded by a few granulosa cells is released into the peritoneal cavity. The nearby uterine tube, either left or correct, receives the oocyte. Unlike sperm, oocytes lack flagella, and therefore cannot move on their own. So how do they travel into the uterine tube and toward the uterus? Loftier concentrations of estrogen that occur around the time of ovulation induce contractions of the polish muscle along the length of the uterine tube. These contractions occur every four to 8 seconds, and the result is a coordinated motility that sweeps the surface of the ovary and the pelvic cavity. Current flowing toward the uterus is generated by coordinated beating of the cilia that line the outside and lumen of the length of the uterine tube. These cilia beat more strongly in response to the high estrogen concentrations that occur effectually the time of ovulation. As a result of these mechanisms, the oocyte–granulosa cell complex is pulled into the interior of the tube. Once inside, the muscular contractions and beating cilia motion the oocyte slowly toward the uterus. When fertilization does occur, sperm typically meet the egg while information technology is notwithstanding moving through the ampulla.
Practice Question
Watch this video to observe ovulation and its initiation in response to the release of FSH and LH from the pituitary gland. What specialized structures help guide the oocyte from the ovary into the uterine tube?
Show Reply
The fimbriae sweep the oocyte into the uterine tube.
If the oocyte is successfully fertilized, the resulting zygote will begin to divide into ii cells, then four, then on, as it makes its mode through the uterine tube and into the uterus. There, it will implant and continue to grow. If the egg is non fertilized, information technology will simply degrade—either in the uterine tube or in the uterus, where information technology may exist shed with the next menstrual period.

Figure 6. This anterior view shows the relationship of the ovaries, uterine tubes (oviducts), and uterus. Sperm enter through the vagina, and fertilization of an ovulated oocyte usually occurs in the distal uterine tube. From left to right, LM × 400, LM × xx. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
The open-concluded structure of the uterine tubes can have significant wellness consequences if leaner or other contagions enter through the vagina and motion through the uterus, into the tubes, and and so into the pelvic crenel. If this is left unchecked, a bacterial infection (sepsis) could apace get life-threatening. The spread of an infection in this manner is of special concern when unskilled practitioners perform abortions in non-sterile weather. Sepsis is too associated with sexually transmitted bacterial infections, especially gonorrhea and chlamydia. These increment a adult female's risk for pelvic inflammatory illness (PID), infection of the uterine tubes or other reproductive organs. Even when resolved, PID can leave scar tissue in the tubes, leading to infertility.
Do Question
Watch this series of videos to look at the movement of the oocyte through the ovary. The cilia in the uterine tube promote motility of the oocyte. What would likely occur if the cilia were paralyzed at the time of ovulation?
Show Answer
The oocyte may not enter the tube and may enter the pelvic cavity.
The Uterus and Cervix
The uterus is the muscular organ that nourishes and supports the growing embryo. Its average size is approximately 5 cm broad past 7 cm long (approximately 2 in by iii in) when a female is not pregnant. It has three sections. The portion of the uterus superior to the opening of the uterine tubes is called the fundus. The middle department of the uterus is called the body of uterus (or corpus). The cervix is the narrow inferior portion of the uterus that projects into the vagina. The neck produces fungus secretions that become sparse and stringy under the influence of high systemic plasma estrogen concentrations, and these secretions can facilitate sperm movement through the reproductive tract.
Several ligaments maintain the position of the uterus inside the abdominopelvic cavity. The wide ligament is a fold of peritoneum that serves as a primary support for the uterus, extending laterally from both sides of the uterus and attaching it to the pelvic wall. The round ligament attaches to the uterus almost the uterine tubes, and extends to the labia majora. Finally, the uterosacral ligament stabilizes the uterus posteriorly by its connection from the cervix to the pelvic wall.
The wall of the uterus is made up of 3 layers. The about superficial layer is the serous membrane, or perimetrium, which consists of epithelial tissue that covers the outside portion of the uterus. The middle layer, or myometrium, is a thick layer of smooth muscle responsible for uterine contractions. Nearly of the uterus is myometrial tissue, and the muscle fibers run horizontally, vertically, and diagonally, allowing the powerful contractions that occur during labor and the less powerful contractions (or cramps) that aid to miscarry menstrual blood during a adult female'southward catamenia. Anteriorly directed myometrial contractions also occur about the time of ovulation, and are thought to mayhap facilitate the transport of sperm through the female person reproductive tract.
The innermost layer of the uterus is called the endometrium. The endometrium contains a connective tissue lining, the lamina propria, which is covered by epithelial tissue that lines the lumen. Structurally, the endometrium consists of ii layers: the stratum basalis and the stratum functionalis (the basal and functional layers). The stratum basalis layer is role of the lamina propria and is adjacent to the myometrium; this layer does not shed during menstruation. In dissimilarity, the thicker stratum functionalis layer contains the glandular portion of the lamina propria and the endothelial tissue that lines the uterine lumen. It is the stratum functionalis that grows and thickens in response to increased levels of estrogen and progesterone. In the luteal phase of the menstrual cycle, special branches off of the uterine artery chosen spiral arteries supply the thickened stratum functionalis. This inner functional layer provides the proper site of implantation for the fertilized egg, and—should fertilization non occur—it is just the stratum functionalis layer of the endometrium that sheds during menstruation.
Recall that during the follicular stage of the ovarian wheel, the tertiary follicles are growing and secreting estrogen. At the same time, the stratum functionalis of the endometrium is thickening to prepare for a potential implantation. The mail service-ovulatory increment in progesterone, which characterizes the luteal phase, is key for maintaining a thick stratum functionalis. As long as a functional corpus luteum is present in the ovary, the endometrial lining is prepared for implantation. Indeed, if an embryo implants, signals are sent to the corpus luteum to keep secreting progesterone to maintain the endometrium, and thus maintain the pregnancy. If an embryo does non implant, no signal is sent to the corpus luteum and it degrades, ceasing progesterone production and ending the luteal stage. Without progesterone, the endometrium thins and, under the influence of prostaglandins, the screw arteries of the endometrium constrict and rupture, preventing oxygenated claret from reaching the endometrial tissue. As a effect, endometrial tissue dies and blood, pieces of the endometrial tissue, and white blood cells are shed through the vagina during menstruation, or the menses. The first flow after puberty, called menarche, tin can occur either earlier or after the first ovulation.
The Menstrual Cycle
Now that nosotros have discussed the maturation of the cohort of tertiary follicles in the ovary, the build-up and then shedding of the endometrial lining in the uterus, and the office of the uterine tubes and vagina, we tin can put everything together to talk about the three phases of the menstrual cycle—the series of changes in which the uterine lining is shed, rebuilds, and prepares for implantation.
The timing of the menstrual cycle starts with the outset day of menstruum, referred to equally solar day one of a adult female'due south period. Bike length is adamant by counting the days between the onset of haemorrhage in two subsequent cycles. Because the average length of a woman'southward menstrual bicycle is 28 days, this is the time period used to identify the timing of events in the bicycle. However, the length of the menstrual cycle varies among women, and even in the same adult female from 1 cycle to the next, typically from 21 to 32 days.
Just every bit the hormones produced by the granulosa and theca cells of the ovary "bulldoze" the follicular and luteal phases of the ovarian cycle, they also control the three distinct phases of the menstrual bike. These are the menses phase, the proliferative phase, and the secretory stage.
Menstruation Stage
The menses phase of the menstrual bike is the phase during which the lining is shed; that is, the days that the woman menstruates. Although it averages approximately five days, the menses phase can last from 2 to vii days, or longer. As shown in Figure 7, the menstruation phase occurs during the early on days of the follicular phase of the ovarian bike, when progesterone, FSH, and LH levels are low. Recollect that progesterone concentrations reject every bit a upshot of the deposition of the corpus luteum, marking the end of the luteal stage. This decline in progesterone triggers the shedding of the stratum functionalis of the endometrium.

Figure 7. Click for a larger image. The correlation of the hormone levels and their effects on the female reproductive system is shown in this timeline of the ovarian and menstrual cycles. The menstrual cycle begins at day one with the start of menstruation. Ovulation occurs around mean solar day fourteen of a 28-twenty-four hour period bicycle, triggered past the LH surge.
Proliferative Phase
In one case menstrual menstruum ceases, the endometrium begins to proliferate again, marker the showtime of the proliferative phase of the menstrual bike. It occurs when the granulosa and theca cells of the 3rd follicles begin to produce increased amounts of estrogen. These rising estrogen concentrations stimulate the endometrial lining to rebuild.
Recall that the high estrogen concentrations will eventually lead to a decrease in FSH as a consequence of negative feedback, resulting in atresia of all but one of the developing tertiary follicles. The switch to positive feedback—which occurs with the elevated estrogen production from the dominant follicle—then stimulates the LH surge that will trigger ovulation. In a typical 28-twenty-four hours menstrual cycle, ovulation occurs on twenty-four hour period 14. Ovulation marks the end of the proliferative stage every bit well as the end of the follicular phase.
Secretory Phase
In addition to prompting the LH surge, high estrogen levels increment the uterine tube contractions that facilitate the pick-up and transfer of the ovulated oocyte. High estrogen levels also slightly decrease the acidity of the vagina, making it more than hospitable to sperm. In the ovary, the luteinization of the granulosa cells of the complanate follicle forms the progesterone-producing corpus luteum, marking the first of the luteal stage of the ovarian cycle. In the uterus, progesterone from the corpus luteum begins the secretory phase of the menstrual wheel, in which the endometrial lining prepares for implantation. Over the next 10 to 12 days, the endometrial glands secrete a fluid rich in glycogen. If fertilization has occurred, this fluid volition nourish the brawl of cells at present developing from the zygote. At the same fourth dimension, the spiral arteries develop to provide blood to the thickened stratum functionalis.
If no pregnancy occurs within approximately 10 to 12 days, the corpus luteum volition dethrone into the corpus albicans. Levels of both estrogen and progesterone will fall, and the endometrium will grow thinner. Prostaglandins will be secreted that cause constriction of the screw arteries, reducing oxygen supply. The endometrial tissue volition die, resulting in menses—or the outset twenty-four hours of the adjacent cycle.
Disorders of the Female person Reproductive Organization
Research over many years has confirmed that cervical cancer is most often caused past a sexually transmitted infection with human papillomavirus (HPV). There are over 100 related viruses in the HPV family unit, and the characteristics of each strain determine the consequence of the infection. In all cases, the virus enters torso cells and uses its ain genetic material to take over the host prison cell's metabolic mechanism and produce more virus particles.
HPV infections are common in both men and women. Indeed, a recent written report determined that 42.5 percent of females had HPV at the fourth dimension of testing. These women ranged in age from xiv to 59 years and differed in race, ethnicity, and number of sexual partners. Of note, the prevalence of HPV infection was 53.eight pct among women aged 20 to 24 years, the historic period grouping with the highest infection rate.
HPV strains are classified every bit loftier or low risk according to their potential to cause cancer. Though virtually HPV infections exercise non crusade disease, the disruption of normal cellular functions in the depression-hazard forms of HPV tin can crusade the male or female person human host to develop genital warts. Often, the trunk is able to clear an HPV infection past normal allowed responses within 2 years. However, the more serious, high-risk infection by certain types of HPV can result in cancer of the cervix. Infection with either of the cancer-causing variants HPV 16 or HPV xviii has been linked to more than seventy percentage of all cervical cancer diagnoses. Although even these high-risk HPV strains can be cleared from the body over time, infections persist in some individuals. If this happens, the HPV infection can influence the cells of the cervix to develop precancerous changes.
Hazard factors for cervical cancer include having unprotected sex; having multiple sexual partners; a get-go sexual experience at a younger age, when the cells of the cervix are not fully mature; failure to receive the HPV vaccine; a compromised immune system; and smoking. The risk of developing cervical cancer is doubled with cigarette smoking.

Effigy eight. In near cases, cells infected with the HPV virus heal on their ain. In some cases, however, the virus continues to spread and becomes an invasive cancer.
When the high-run a risk types of HPV enter a cell, two viral proteins are used to neutralize proteins that the host cells use as checkpoints in the cell bike. The best studied of these proteins is p53. In a normal cell, p53 detects Deoxyribonucleic acid damage in the cell's genome and either halts the progression of the cell bike—allowing fourth dimension for DNA repair to occur—or initiates apoptosis. Both of these processes foreclose the accumulation of mutations in a cell's genome. High-risk HPV can neutralize p53, keeping the cell in a state in which fast growth is possible and impairing apoptosis, assuasive mutations to accumulate in the cellular Deoxyribonucleic acid.
The prevalence of cervical cancer in the United States is very low considering of regular screening exams called pap smears. Pap smears sample cells of the cervix, allowing the detection of abnormal cells. If pre-cancerous cells are detected, at that place are several highly effective techniques that are currently in use to remove them before they pose a danger. Nonetheless, women in developing countries often practice not take admission to regular pap smears. As a result, these women account for as many as eighty percent of the cases of cervical cancer worldwide.
In 2006, the first vaccine against the high-risk types of HPV was approved. There are now two HPV vaccines available: Gardasil® and Cervarix®. Whereas these vaccines were initially just targeted for women, considering HPV is sexually transmitted, both men and women require vaccination for this arroyo to achieve its maximum efficacy. A contempo study suggests that the HPV vaccine has cut the rates of HPV infection by the four targeted strains at least in half. Unfortunately, the high price of manufacturing the vaccine is currently limiting access to many women worldwide.
The Breasts
Whereas the breasts are located far from the other female reproductive organs, they are considered accompaniment organs of the female reproductive organisation. The function of the breasts is to supply milk to an baby in a process called lactation. The external features of the chest include a nipple surrounded past a pigmented areola, whose coloration may deepen during pregnancy. The areola is typically round and tin can vary in size from 25 to 100 mm in diameter. The areolar region is characterized by small, raised areolar glands that secrete lubricating fluid during lactation to protect the nipple from chafing. When a baby nurses, or draws milk from the breast, the entire areolar region is taken into the oral fissure.
Breast milk is produced past the mammary glands, which are modified sweat glands. The milk itself exits the chest through the nipple via xv to twenty lactiferous ducts that open on the surface of the nipple. These lactiferous ducts each extend to a lactiferous sinus that connects to a glandular lobe inside the breast itself that contains groups of milk-secreting cells in clusters called alveoli. The clusters tin can change in size depending on the amount of milk in the alveolar lumen. Once milk is fabricated in the alveoli, stimulated myoepithelial cells that surround the alveoli contract to push the milk to the lactiferous sinuses. From hither, the baby can describe milk through the lactiferous ducts by suckling. The lobes themselves are surrounded past fat tissue, which determines the size of the chest; breast size differs between individuals and does not touch the amount of milk produced. Supporting the breasts are multiple bands of connective tissue chosen suspensory ligaments that connect the breast tissue to the dermis of the overlying peel.

Figure 9. During lactation, milk moves from the alveoli through the lactiferous ducts to the nipple.
During the normal hormonal fluctuations in the menstrual cycle, breast tissue responds to changing levels of estrogen and progesterone, which can lead to swelling and breast tenderness in some individuals, especially during the secretory phase. If pregnancy occurs, the increase in hormones leads to further development of the mammary tissue and enlargement of the breasts.
Hormonal Birth Control
Nascence command pills take reward of the negative feedback system that regulates the ovarian and menstrual cycles to terminate ovulation and preclude pregnancy. Typically they work by providing a constant level of both estrogen and progesterone, which negatively feeds dorsum onto the hypothalamus and pituitary, thus preventing the release of FSH and LH. Without FSH, the follicles practise non mature, and without the LH surge, ovulation does not occur. Although the estrogen in nativity control pills does stimulate some thickening of the endometrial wall, it is reduced compared with a normal bike and is less likely to support implantation.
Some birth control pills contain 21 active pills containing hormones, and seven inactive pills (placebos). The decline in hormones during the week that the adult female takes the placebo pills triggers menses, although it is typically lighter than a normal menstrual flow because of the reduced endometrial thickening. Newer types of nascency control pills accept been developed that deliver depression-dose estrogens and progesterone for the entire cycle (these are meant to exist taken 365 days a year), and period never occurs. While some women prefer to have the proof of a lack of pregnancy that a monthly period provides, menstruum every 28 days is non required for health reasons, and at that place are no reported adverse effects of not having a menstrual period in an otherwise salubrious private.
Because nativity control pills office past providing constant estrogen and progesterone levels and disrupting negative feedback, skipping even merely 1 or 2 pills at certain points of the bicycle (or even existence several hours late taking the pill) can atomic number 82 to an increase in FSH and LH and result in ovulation. It is important, therefore, that the adult female follow the directions on the birth control pill packet to successfully preclude pregnancy.
Aging and the Female Reproductive System
Female fertility (the power to conceive) peaks when women are in their twenties, and is slowly reduced until a women reaches 35 years of age. Later on that time, fertility declines more than speedily, until it ends completely at the end of menopause. Menopause is the cessation of the menstrual cycle that occurs as a issue of the loss of ovarian follicles and the hormones that they produce. A woman is considered to take completed menopause if she has not menstruated in a full year. Later that point, she is considered postmenopausal. The average age for this change is consistent worldwide at betwixt fifty and 52 years of historic period, just it tin can commonly occur in a woman's forties, or later in her fifties. Poor health, including smoking, tin atomic number 82 to before loss of fertility and earlier menopause.
Every bit a woman reaches the age of menopause, depletion of the number of feasible follicles in the ovaries due to atresia affects the hormonal regulation of the menstrual cycle. During the years leading upwardly to menopause, there is a decrease in the levels of the hormone inhibin, which commonly participates in a negative feedback loop to the pituitary to control the production of FSH. The menopausal decrease in inhibin leads to an increase in FSH. The presence of FSH stimulates more follicles to abound and secrete estrogen. Because small, secondary follicles as well respond to increases in FSH levels, larger numbers of follicles are stimulated to grow; still, most undergo atresia and die. Eventually, this process leads to the depletion of all follicles in the ovaries, and the production of estrogen falls off dramatically. It is primarily the lack of estrogens that leads to the symptoms of menopause.
The primeval changes occur during the menopausal transition, oftentimes referred to as peri-menopause, when a women's cycle becomes irregular just does non end entirely. Although the levels of estrogen are notwithstanding virtually the same every bit before the transition, the level of progesterone produced by the corpus luteum is reduced. This decline in progesterone tin can pb to abnormal growth, or hyperplasia, of the endometrium. This condition is a business organisation because information technology increases the chance of developing endometrial cancer. Two harmless conditions that tin can develop during the transition are uterine fibroids, which are benign masses of cells, and irregular bleeding. As estrogen levels modify, other symptoms that occur are hot flashes and night sweats, trouble sleeping, vaginal dryness, mood swings, difficulty focusing, and thinning of pilus on the head along with the growth of more hair on the face. Depending on the private, these symptoms tin be entirely absent, moderate, or severe.
After menopause, lower amounts of estrogens can lead to other changes. Cardiovascular affliction becomes as prevalent in women as in men, possibly because estrogens reduce the amount of cholesterol in the blood vessels. When estrogen is lacking, many women find that they of a sudden have bug with high cholesterol and the cardiovascular issues that accompany information technology. Osteoporosis is another problem because os density decreases speedily in the first years subsequently menopause. The reduction in bone density leads to a higher incidence of fractures.
Hormone therapy (HT), which employs medication (constructed estrogens and progestins) to increase estrogen and progestin levels, tin alleviate some of the symptoms of menopause. In 2002, the Women's Health Initiative began a study to observe women for the long-term outcomes of hormone replacement therapy over 8.5 years. However, the study was prematurely terminated after five.2 years because of prove of a college than normal chance of breast cancer in patients taking estrogen-simply HT. The potential positive effects on cardiovascular illness were also non realized in the estrogen-simply patients. The results of other hormone replacement studies over the last 50 years, including a 2012 study that followed over ane,000 menopausal women for 10 years, accept shown cardiovascular benefits from estrogen and no increased risk for cancer. Some researchers believe that the age group tested in the 2002 trial may take been too onetime to benefit from the therapy, thus skewing the results. In the meantime, intense debate and report of the benefits and risks of replacement therapy is ongoing. Current guidelines approve HT for the reduction of hot flashes or flushes, merely this handling is mostly simply considered when women first offset showing signs of menopausal changes, is used in the lowest dose possible for the shortest time possible (5 years or less), and it is suggested that women on HT take regular pelvic and breast exams.
Chapter Review
The external female ballocks are collectively chosen the vulva. The vagina is the pathway into and out of the uterus. The human'south penis is inserted into the vagina to deliver sperm, and the baby exits the uterus through the vagina during childbirth.
The ovaries produce oocytes, the female gametes, in a process called oogenesis. As with spermatogenesis, meiosis produces the haploid gamete (in this case, an ovum); however, it is completed merely in an oocyte that has been penetrated past a sperm. In the ovary, an oocyte surrounded past supporting cells is chosen a follicle. In folliculogenesis, primordial follicles develop into primary, secondary, and third follicles. Early tertiary follicles with their fluid-filled antrum will be stimulated by an increase in FSH, a gonadotropin produced by the inductive pituitary, to grow in the 28-day ovarian bicycle. Supporting granulosa and theca cells in the growing follicles produce estrogens, until the level of estrogen in the bloodstream is high enough that it triggers negative feedback at the hypothalamus and pituitary. This results in a reduction of FSH and LH, and most tertiary follicles in the ovary undergo atresia (they die). One follicle, normally the one with the most FSH receptors, survives this period and is now called the ascendant follicle. The dominant follicle produces more estrogen, triggering positive feedback and the LH surge that volition induce ovulation. Following ovulation, the granulosa cells of the empty follicle luteinize and transform into the progesterone-producing corpus luteum. The ovulated oocyte with its surrounding granulosa cells is picked upward past the infundibulum of the uterine tube, and chirapsia cilia assist to send information technology through the tube toward the uterus. Fertilization occurs inside the uterine tube, and the final stage of meiosis is completed.
The uterus has 3 regions: the fundus, the body, and the cervix. Information technology has three layers: the outer perimetrium, the muscular myometrium, and the inner endometrium. The endometrium responds to estrogen released by the follicles during the menstrual bicycle and grows thicker with an increase in blood vessels in preparation for pregnancy. If the egg is non fertilized, no signal is sent to extend the life of the corpus luteum, and it degrades, stopping progesterone product. This decline in progesterone results in the sloughing of the inner portion of the endometrium in a process called menses, or catamenia.
The breasts are accompaniment sexual organs that are utilized after the nascence of a child to produce milk in a process called lactation. Nascency command pills provide constant levels of estrogen and progesterone to negatively feed dorsum on the hypothalamus and pituitary, and suppress the release of FSH and LH, which inhibits ovulation and prevents pregnancy.
Self Check
Answer the question(southward) below to meet how well you understand the topics covered in the previous department.
Critical Thinking Questions
- Follow the path of ejaculated sperm from the vagina to the oocyte. Include all structures of the female reproductive tract that the sperm must swim through to reach the egg.
- Identify some differences between meiosis in men and women.
- Explain the hormonal regulation of the phases of the menstrual cycle.
- Endometriosis is a disorder in which endometrial cells implant and proliferate outside of the uterus—in the uterine tubes, on the ovaries, or even in the pelvic cavity. Offer a theory every bit to why endometriosis increases a woman's risk of infertility.
Glossary
alveoli: (of the breast) milk-secreting cells in the mammary gland
ampulla: (of the uterine tube) middle portion of the uterine tube in which fertilization often occurs
antrum: fluid-filled chamber that characterizes a mature tertiary (antral) follicle
areola: highly pigmented, circular surface area surrounding the raised nipple and containing areolar glands that secrete fluid of import for lubrication during suckling
Bartholin's glands: (also, greater vestibular glands) glands that produce a thick mucus that maintains moisture in the vulva area; also referred to every bit the greater vestibular glands
torso of uterus: heart section of the uterus
broad ligament: wide ligament that supports the uterus by attaching laterally to both sides of the uterus and pelvic wall
cervix: elongate inferior end of the uterus where it connects to the vagina
clitoris: (also, glans clitoris) nervus-rich area of the vulva that contributes to sexual sensation during intercourse
corpus albicans: nonfunctional structure remaining in the ovarian stroma post-obit structural and functional regression of the corpus luteum
corpus luteum: transformed follicle after ovulation that secretes progesterone
endometrium: inner lining of the uterus, part of which builds up during the secretory phase of the menstrual cycle and and so sheds with menses
fimbriae: fingerlike projections on the distal uterine tubes
follicle: ovarian structure of one oocyte and surrounding granulosa (and later on theca) cells
folliculogenesis: development of ovarian follicles from primordial to 3rd under the stimulation of gonadotropins
fundus: (of the uterus) domed portion of the uterus that is superior to the uterine tubes
granulosa cells: supportive cells in the ovarian follicle that produce estrogen
hymen: membrane that covers part of the opening of the vagina
infundibulum: (of the uterine tube) wide, distal portion of the uterine tube terminating in fimbriae
isthmus: narrow, medial portion of the uterine tube that joins the uterus
labia majora: hair-covered folds of skin located behind the mons pubis
labia minora: thin, pigmented, hairless flaps of skin located medial and deep to the labia majora
lactiferous ducts: ducts that connect the mammary glands to the nipple and allow for the ship of milk
lactiferous sinus: area of milk collection between alveoli and lactiferous duct
mammary glands: glands inside the breast that secrete milk
menarche: beginning menses in a pubertal female
menstruum: shedding of the inner portion of the endometrium out though the vagina; also referred to as flow
menses phase: stage of the menstrual cycle in which the endometrial lining is shed
menstrual cycle: approximately 28-twenty-four hour period bicycle of changes in the uterus consisting of a menses stage, a proliferative stage, and a secretory phase
mons pubis: mound of fat tissue located at the front of the vulva
myometrium: polish musculus layer of uterus that allows for uterine contractions during labor and expulsion of menstrual blood
oocyte: prison cell that results from the division of the oogonium and undergoes meiosis I at the LH surge and meiosis II at fertilization to become a haploid ovum
oogenesis: process by which oogonia divide by mitosis to main oocytes, which undergo meiosis to produce the secondary oocyte and, upon fertilization, the ovum
oogonia: ovarian stem cells that undergo mitosis during female fetal development to form master oocytes
ovarian bicycle: approximately 28-day cycle of changes in the ovary consisting of a follicular phase and a luteal stage
ovaries: female person gonads that produce oocytes and sex activity steroid hormones (notably estrogen and progesterone)
ovulation: release of a secondary oocyte and associated granulosa cells from an ovary
ovum: haploid female person gamete resulting from completion of meiosis 2 at fertilization
perimetrium: outer epithelial layer of uterine wall
polar body: smaller jail cell produced during the process of meiosis in oogenesis
primary follicles: ovarian follicles with a master oocyte and one layer of cuboidal granulosa cells
primordial follicles: least developed ovarian follicles that consist of a single oocyte and a single layer of apartment (squamous) granulosa cells
proliferative phase: phase of the menstrual wheel in which the endometrium proliferates
rugae: (of the vagina) folds of skin in the vagina that permit it to stretch during intercourse and childbirth
secondary follicles: ovarian follicles with a chief oocyte and multiple layers of granulosa cells
secretory stage: stage of the menstrual wheel in which the endometrium secretes a nutrient-rich fluid in grooming for implantation of an embryo
suspensory ligaments: bands of connective tissue that suspend the breast onto the chest wall by attachment to the overlying dermis
tertiary follicles: (as well, antral follicles) ovarian follicles with a primary or secondary oocyte, multiple layers of granulosa cells, and a fully formed antrum
theca cells: estrogen-producing cells in a maturing ovarian follicle
uterine tubes: (also, fallopian tubes or oviducts) ducts that facilitate transport of an ovulated oocyte to the uterus
uterus: muscular hollow organ in which a fertilized egg develops into a fetus
vagina: tunnel-like organ that provides access to the uterus for the insertion of semen and from the uterus for the nascency of a baby
vulva: external female ballocks
Source: https://courses.lumenlearning.com/suny-ap2/chapter/anatomy-and-physiology-of-the-female-reproductive-system/
0 Response to "Artlabeling Activity Ovaries and Their Relationship to the Uterine Tubes and Uterus 1 of 2"
Post a Comment